- CBCT generates detailed 3-D imaging of the TMJs.
- Case selection for TMJ imaging is essential since not all TMD issues are detectable on CBCT.
- A thorough understanding of TMD and normal TMJ anatomy leads to an appropriate diagnosis.
- CBCT Reports provided via Oral & Maxillofacial Radiologists’ interpretation ensures proper documentation of TMD as well as all incidental findings within CBCT scans.
Cone-beam computed tomography (CBCT) is a fantastic diagnostic imaging modality for evaluation of temporomandibular joint disorders (TMD). Some key considerations will be detailed for CBCT interpretation with respect to TMD.
TMD is a common condition that affects the temporomandibular joint (TMJ) – the joint that connects the mandible (lower) jaw to the skull. This condition can cause pain, clicking or popping sounds when opening and closing the mouth, and difficulty in jaw movement. CBCT can help to identify the structural and functional abnormalities that contribute to TMD.
Clinicians must be aware of the normal anatomy and function of the TMJ, which will help them more easily recognize abnormalities. The patient’s symptoms and clinical history must first be gathered to first determine the need for imaging and will also facilitate proper correlation of the imaging findings with the patient’s clinical presentation. It should be noted that there are limitations of CBCT imaging, and while CBCT provides detailed anatomical information, it does not reveal functional information about the TMJ. Oftentimes, functional disorders can be clinically diagnosed without the need for advanced imaging like CBCT, CT, or MRI.
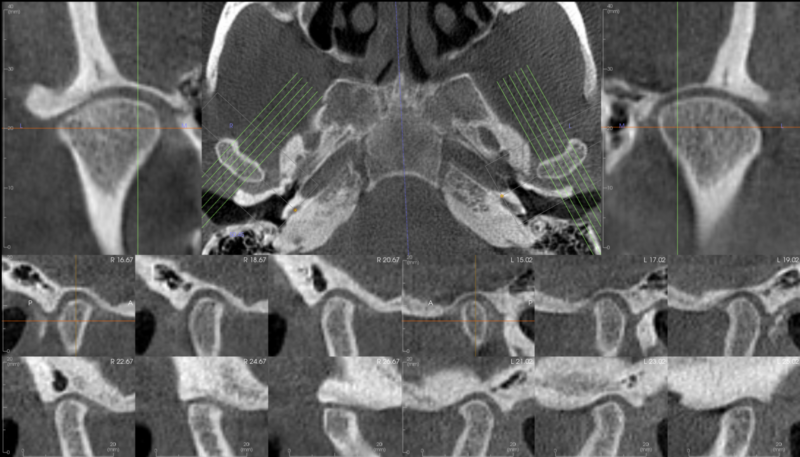
After selecting the appropriate volume size, the CBCT scan generates three-dimensional images of the TMJ anatomy. A quality TMJ series includes the mandibular condyles, articular eminences of the temporal bone, and the joint spaces – these should be included in both a closed and open scan, the closed with the patient’s teeth together in centric occlusion and the open in maximum open position.
It is critical to understand that the temporomandibular disc itself will not be depicted, as the low radiation dose for patients from CBCT studies comes at the expense of soft tissue contrast. Acquiring a second study with the patient’s mouth wide open and comparing the relative position of the condyles and articular eminences may allow some inference as to the disc position. Yet another study in a different excursive position may be useful. Any additional study should be acquired with the lowest possible radiation dose for the patient. For practices frequently acquiring multiple CBCT studies for each case, utilizing a machine with Ultra Low-Dose parameter capabilities is advised. If it is imperative the disc and capsular ligaments be visualized in imaging, both MDCT and MRI studies will depict it, often acquired with a contrast medium.
Once the scan is complete, the images are viewed within software that can display the DICOM file type. Most imaging software provides tools for measuring joint space, disc position, and bone morphology, as well as tools for modifying contrast, brightness, sharpness, and many other settings to enhance visualization and interpretation.
TMJ pathology can be bilateral but is oftentimes unilateral. The most common pathologic CBCT finding involving the bones of the TMJ is degenerative joint disease, in which the cortices are thin, irregular, and often interrupted. There may be sclerosis of the underlying trabecular bone due to inflammation. When there is condylar volume loss, the condyle may be short vertically and/or narrow in the anterior-posterior or even the mediolateral dimension. If detected early, one or both condyles may just exhibit mild flattening and cortical thinning.
Other conditions that may be occasionally detected include additional inflammatory diseases like Progressive Condylar Resorption, the demographic for which is almost exclusively young females, and the autoimmune disorder Rheumatoid Arthritis. Some tumors include osteochondroma (benign) and osteosarcoma and chondrosarcoma (both malignant). Hyperplasia is another benign condition that can be present, notable by an elongated condylar neck. Hyperplasia of the coronoid process can also occur, which may impact wide mouth opening due to mechanical interference between the coronoid process and zygomatic process.
With careful interpretation and appropriate case selection, CBCT can provide important information for the diagnosis and treatment planning of TMD. To help practices properly diagnose and document findings related to TMD via official radiology reports (CBCT Reports), Oral & Maxillofacial Radiologists’ specialty expertise should be utilized via HIPAA-safe transfer of the CBCT DICOMS.