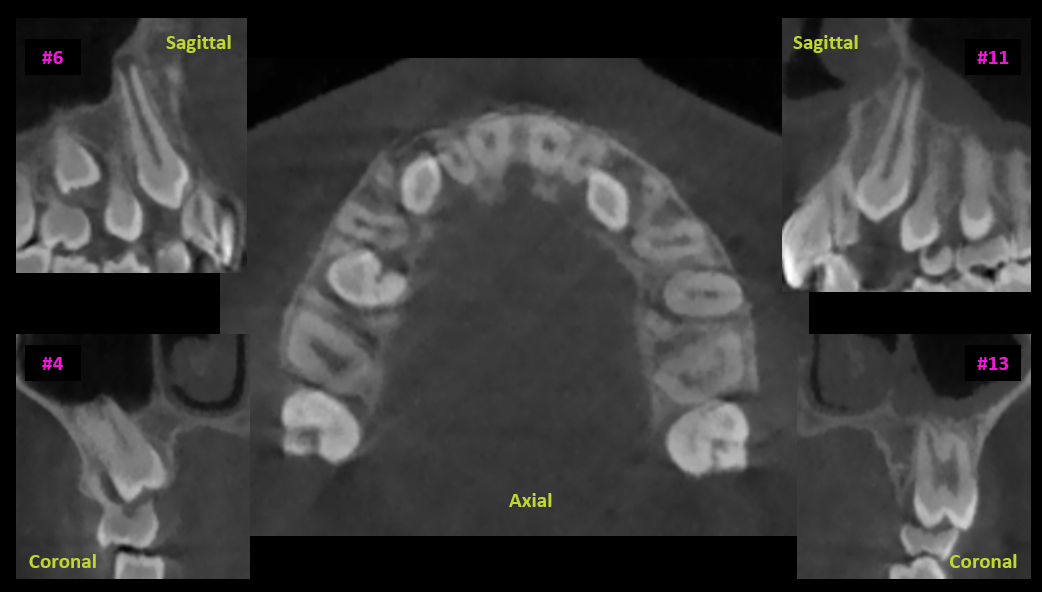
- CBCT can depict impacted teeth and the structures surrounding them prior to any intervention.
- Identification and preservation of critical anatomy is essential for maintaining quality of life.
- When used appropriately, data from CBCT images will affect treatment and enhance outcomes.
- Oral & Maxillofacial Radiologists’ official CBCT Reports provide detailed descriptions of the effects impacted teeth have on critical anatomy, facilitating enhanced risk analysis by the clinician.
Cone Beam Computed Tomography (CBCT) is a modern radiographic technique that generates 3-D images of the jaw, teeth, and surrounding structures. This technology has revolutionized the field of dentistry, allowing for accurate diagnosis and treatment planning, including impacted teeth.
An impacted tooth remains at least partially unerupted in the maxilla or mandible with no realistic chance of eruption into the arch. Causes for this condition vary, but most commonly it is due to the position or orientation of the tooth precluding proper eruption, the arch length is insufficient, a different permanent or retained primary tooth is obstructing, or some pathology associated with the impacted tooth or in its path of eruption. There are even a myriad of syndromes that exhibit impacted teeth as one of their most recognizable radiographic features.
An impacted tooth can be innocuous, but it also has the potential to create a range of issues, some of which are severe. Cysts and tumors of the jaws can develop from the follicle surrounding an impacted tooth. Infection can result, as well as damage to adjacent teeth through a process called resorption. Conventional imaging like panoramic and periapical radiographs are two-dimensional, so do not provide enough information to accurately depict the regional anatomy. CBCT scans provide a three-dimensional view of the area of interest, providing certainty regarding tooth position and the surrounding anatomical structures.
Some of the more critical anatomic structures to identify include the regional neurovascular bundles. The inferior alveolar nerve canal (IAN, or ‘mandibular’ canal) enters the mandible on the medial aspect of the ramus through the mandibular foramen. The mental nerve branches from it in the mandibular premolar region, curving laterally to exit the mandible through the mental foramen. The posterior superior alveolar artery (PSAA) canal enters the maxilla from the pterygopalatine fossa at approximately the mid-height of the maxillary sinus through its posterior wall. The greater and lesser palatine foramina are in the posterolateral aspects of the palate, and the incisive canal in the anteromedial aspect of the palate. As their contents include arterial blood and sensory innervation, damaging them can be catastrophic. Pre-operative awareness of their position relative to the impacted teeth can certainly enhance their preservation, and in some cases, treatment protocols can be modified to minimize, if not eliminate, this risk.
When pathology is suspected based on the CBCT imaging results, appropriate management can be implemented. Some conditions may present needing urgent intervention, such as pain from acute inflammation around an impacted tooth. Other situations may call for a methodical approach with need for additional imaging, biopsy, and narrowing a differential diagnosis, as would be the case when a pericoronal tumor like ameloblastoma is suspected. Wherever the situation lies on that spectrum, the appropriate interpretation of the CBCT images will have significant influence on clinical management decisions.
Every dental practice should have radiographic imaging protocols in place for the various situations that present, and should be tailored to conditions, not profiles. For example, every 17-year-old new patient does not necessarily require a CBCT scan to assess their wisdom teeth. But, if a 17-year-old new patient has a panoramic radiograph that depicts superimposition of the IAN canals over the impacted mandibular third molars, this patient is a great candidate for a CBCT scan – in accordance with As Low as Diagnostically Acceptable (ALADA), one must consider using a medium or small-sized field-of-view (FOV) depending on whether this nearness to critical anatomy condition exists bilaterally or unilaterally. This custom approach will promote accurate diagnosis and set the stage for appropriate case selection and treatment planning.