MRI (TMJ) Imaging
MRI FAQs
- What is MRI and how is it different from CBCT?
- Magnetic Resonance Imaging (MRI) uses a strong magnetic field and radio waves to generate 3-D images vs. ionizing radiation of CBCT (note: radiation for CBCT is substantially lower than medical CT imaging).
- Besides no radiation exposure, what are the benefits of MRI (TMJ)?
- In addition to no biological risk, MRI offers exceptional soft tissue imaging to determine the extent of Temporomandibular Joint Disorders (TMD).
- What are the downsides / risks of MRI?
- Claustrophobia – exam requires patients to lay in a somewhat enclosed space for an extended period (30 minutes) vs. the brevity and standing position of CBCT.
- Medical devices – metal-containing ones may malfunction or dislodge during the exam. The MRI Imaging Center will pre-screen to ensure safety.
- Should I have my patient’s braces removed prior to an MRI (TMJ) analysis? And what about their implants?
- Since braces and implants do not dislodge, there is no safety concern. However, stainless steel brackets may potentially lead to non-diagnostic imaging (due to “magnetic susceptibility artifact”). If ceramic or titanium brackets, simply removing the stainless-steel archwire should suffice (but not needed if Ni-Ti, Co-Cr, or Ti-Mb arch wire).
- My patient is pregnant. Can she get an MRI? And, what about the use of intravenous contrast agent during pregnancy?
- There is a large consensus that MRI is safe throughout the entire pregnancy, but MRI Imaging Centers will typically limit non-emergency scans to the first trimester out of an abundance of caution. Note this decision is usually case-by-case after consultation with the patient’s physician.
- Gadolinium is the contrast agent used in MRI and should be avoided during pregnancy (unless absolutely needed) given the association with stillbirth, neonatal death, inflammatory, rheumatological, and infiltrative conditions.
- Which types of medical devices are not allowed with MRI?
- Insulin pumps, ventricular assist devices, LINX Reflux Management System, “Triggerfish” contact lenses, pulmonary artery monitoring catheters, and temporary transvenous pacing leads. The MRI Imaging Center will pre-screen to ensure safety.
MRI Fundamentals
- Larmor (processional) frequency: Measure of the rate of procession of hydrogen atom magnetic dipole moments around an external magnetic field
- If the radio wave pulse is at the same value as Larmor frequency, hydrogen atom resonance occurs (larger amplitude) causing a change in angle of procession
- If magnetic field increases, resonance frequency, signal-to-noise ratio, and T1 increases; however, no change in T2
Spin Echo (SE) Sequence
- Slice encoding gradient + 90° pulse
- Phase encoding gradient
- Slice encoding gradient + 180° pulse
- Frequency encoding gradient + Echo signal
Determining Factors (TR and TE) for SE Image Contrast
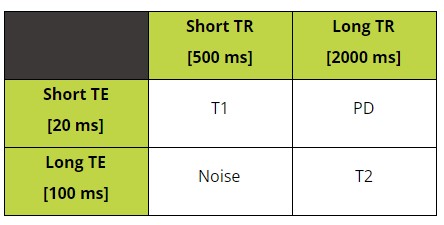
T1 Series
- Brain looks like it’s supposed to (inner white matter brighter than outer grey matter)
- Fat is bright
- Good for detecting Lipomas
T1 (+ Contrast agent) Series
- Turbinates / Septum / Vessels enhanced
- Contrast agent
- Gadolinium (Gd-DTPA) enhances T1 contrast in the arterial phase
- Disrupts local magnetic field
- Increases Specificity of low-Sensitivity MRI scans
T2 Series
- Fluid is bright (Eyes, CSF)
- Good for detecting Cysts, Myxoma, and Joint Effusion
- Fat is less bright than T1 (but still bright!)
PD Series
- Highest Signal-to-Noise Ratio
- Due to differences in number of magnetized protons per unit volume of tissue
- Good for detecting Disc perforation
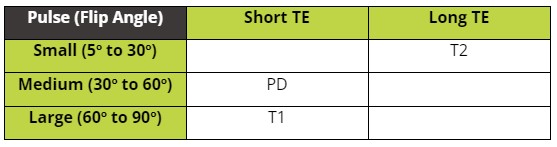
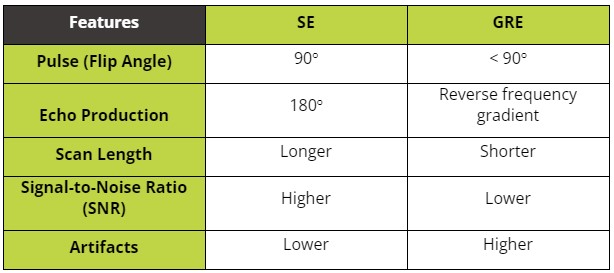
Gradient Recalled Echo (GRE) Sequence
- Unlike SE, 180° pulse not used to avoid inversion of the longitudinal magnetization vector
Determining factors (TE and Flip Angle) for GRE image contrast
Comparison between SE and GRE
Inversion Recovery Sequence
- Slice encoding gradient + 180° pulse
- Slice encoding gradient + 90° pulse
- Phase encoding gradient
- Slice encoding gradient + 180° pulse
- Frequency encoding gradient + Echo signal
- Inversion recovery deploys a preparatory pulse that affects all protons in the imaging field and relies on the specific longitudinal recovery rates of the targeted tissue to reach the desired signal-nulling effect
STIR Series
- Inversion recovery set to null fat signal
- Removes fast relaxation proton signal
- Good for highlighting effect of contrast agent
FLAIR (T2*) Series
- Inversion recovery set to null fluid signal
- Removes slow relaxation proton signal
- Good for calcifications and hemorrhage (dark “blooming” artifact)
- Good for detecting Multiple Sclerosis
MRI Random Facts
Voxel Calculation
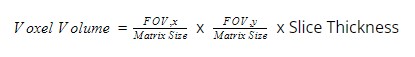
Example: FOV is 20 cm x 20 cm, 4 mm slice thickness, and 320 x 320 matrix
Slice Thickness
- Pulse bandwidth (keeping gradient strength constant)
- Narrow bandwidth, then thinner slice
- Gradient strength (keeping pulse bandwidth constant)
- Steeper slope (higher amplitude), then thinner slice
- Angle of Gradient coil
- More angle, then thinner slice
Artifacts
- Drop Signal: Very low signal in the middle of a high signal lesion
- Signal Void: Same appearance as Drop Signal, but within a vessels
- Chemical Shift: Curvilinear hyperintensity signal adjacent to low signal at a tissue-tissue interface – due to difference in resonance frequency of fat vs. water protons and occurs in the frequency-encoding gradient
- Magnetic Susceptibility: Very low signal from metal (due to rapid dephasing) – common cause in the maxillofacial region is metallic restorations, implants, and orthodontic brackets
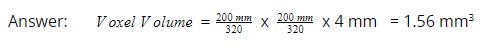
How to Age Trauma-induced Blood within the Brain Parenchyma
Help Center
Check out the Help Center for Instructions and FAQs.
Community Impact
Help us give back by suggesting causes that matter to you.
Contact Us for Support
Have a question the Help Center did not answer?