Authors:
Ashwini Bhangale, BDS
Rutgers School of Dental Medicine, Newark, New Jersey, USA
Pranav Parasher, BDS
Rutgers School of Dental Medicine, Newark, New Jersey, USA
Dr. Adriana Creanga, BDS, MS
Rutgers School of Dental Medicine, Newark, New Jersey, USA
Case History
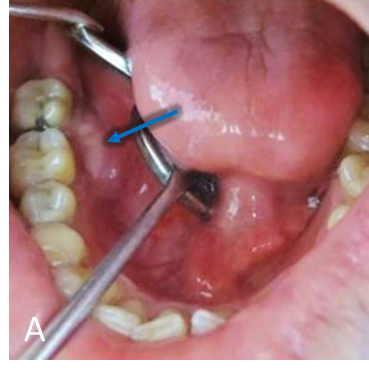
A 30-year-old male patient presented with the chief complaint of swelling in the right second molar area for past 7 months (Figure A, blue arrow).
Imaging
Figure Legend
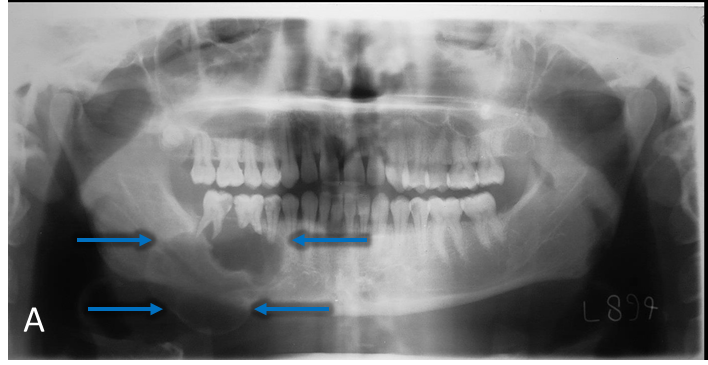
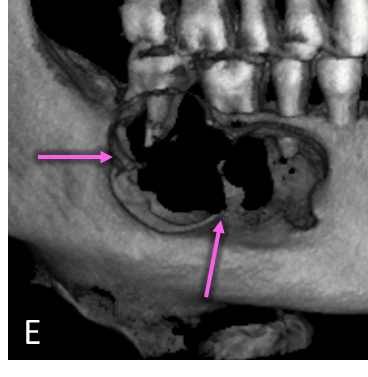
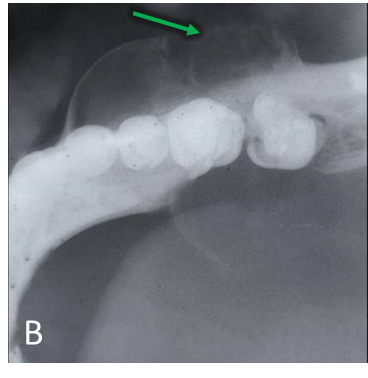
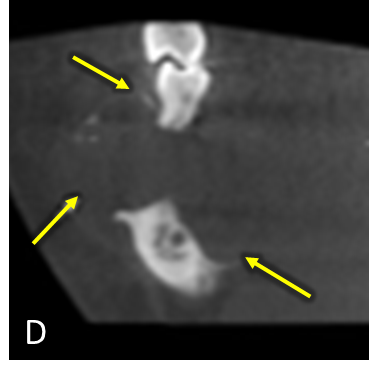
Panoramic radiograph (A) demonstrates a multilocular, well-defined, partially corticated, radiolucent lesion in the mandibular right posterior region (blue arrow). Lesion extends anterior-posteriorly from #28 to #31 and occupies the superior two-thirds of the mandibular body. Lesion is causing interruption of the alveolar crest and external root resorption of #29-31. Mandibular canal is mildly displaced near the anterior aspect of the lesion. Lateral occlusal radiograph (B) demonstrates a multilocular radiolucent lesion in the premolar-molar region (green arrow). Lesion is causing expansion and interruption of the buccal and lingual cortices with lingual displacement of #31. Axial CBCT (C) demonstrates expansion and interruption of the buccal and lingual cortical plates (red arrows). Coronal CBCT (D) demonstrates expansion and interruption of the alveolar crest and the buccal and lingual mandibular cortices (yellow arrows). CBCT 3D Reconstruction (E) demonstrates locular internal borders (pink arrow).
Diagnosis
Impression (Lesion Category)
Benign Neoplasm, Odontogenic
Differential Diagnosis
Ameloblastoma
- Multilocular, extensive buccal/lingual expansion and root resorption
Odontogenic Keratocyst
- Less likely because of the expansion profile – usually anterior-posteriorly
Odontogenic Myxoma
- Less likely because there are no straight septae within the lesion
Final Diagnosis
Ameloblastoma
Summary
Key Radiographic Features vs. Case Findings
Location
- Posterior mandible – typical of Ameloblastoma 80% of the time
- Note: If lesion was located more posteriorly, Ameloblastoma tends to spare the mandibular angle
Periphery and Shape
- Non-uniform buccal & lingual expansion, thinning (“eggshell”), and perforation of the cortices – all typical of Ameloblastoma
Effects on Surrounding Structures
- Teeth: Displaced, “knife-edged” root resorption – typical pattern of Ameloblastoma
- Mandibular canal: Displaced – minimal due to location
Internal Structure
- Low density with curved septa (“soap bubble” or “spider web” loculations) – typical pattern of Ameloblastoma
Management
Biopsy
- Incisional due to Benign Neoplasm impression unlikely to be of vascular origin
Advanced Imaging
- MDCT to determine surgical margins and effect on surrounding soft tissues
Surgical / Treatment Options
- En bloc resection and mandibular reconstruction
Biopsy / Histopathology / Follow-up Legend
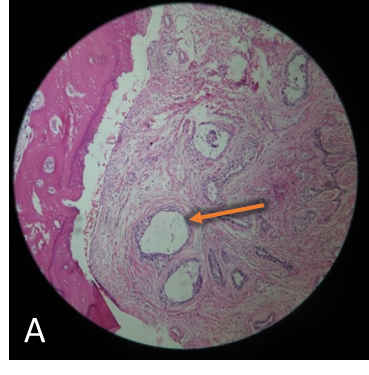
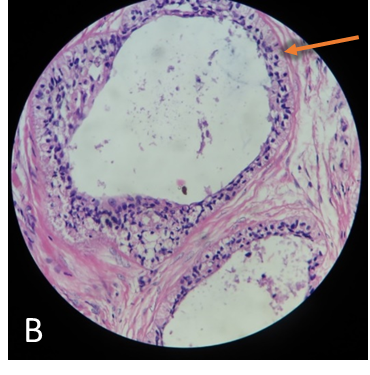
Histopathological slides with hematoxylin-eosin staining (A, B) show characteristic appearance of Follicular Ameloblastoma i.e., microcytic formations with peripheral hyperchromatic and reverse polarity cells (orange arrows).
Suggested Readings
- White, Stuart C., and M. J. Pharoah. Oral Radiology: Principles and Interpretation. Elsevier, 2014.
- Becelli, R., et al. “Mandibular Ameloblastoma: Analysis of Surgical Treatment Carried out in 60 Patients between 1977 and 1998.” Journal of Craniofacial Surgery, vol. 13, no. 3, 2002, pp. 395–400., https://doi.org/10.1097/00001665-200205000-00006.
- Dunfee, Brian L., et al. “Radiologic and Pathologic Characteristics of Benign and Malignant Lesions of the Mandible.” RadioGraphics, vol. 26, no. 6, 2006, pp. 1751–1768., https://doi.org/10.1148/rg.266055189.